Introduction
In recent years, infrared thermography (IRT) has gained recognition as a valuable tool in the field of physical rehabilitation. It offers a non-invasive, contact-free, and radiation-free method for observing physiological responses by capturing thermal emissions from the surface of the skin. Unlike conventional imaging techniques, which focus on anatomical abnormalities, IRT provides a visual representation of functional physiological changes—notably those associated with blood flow, inflammation, and musculoskeletal stress.
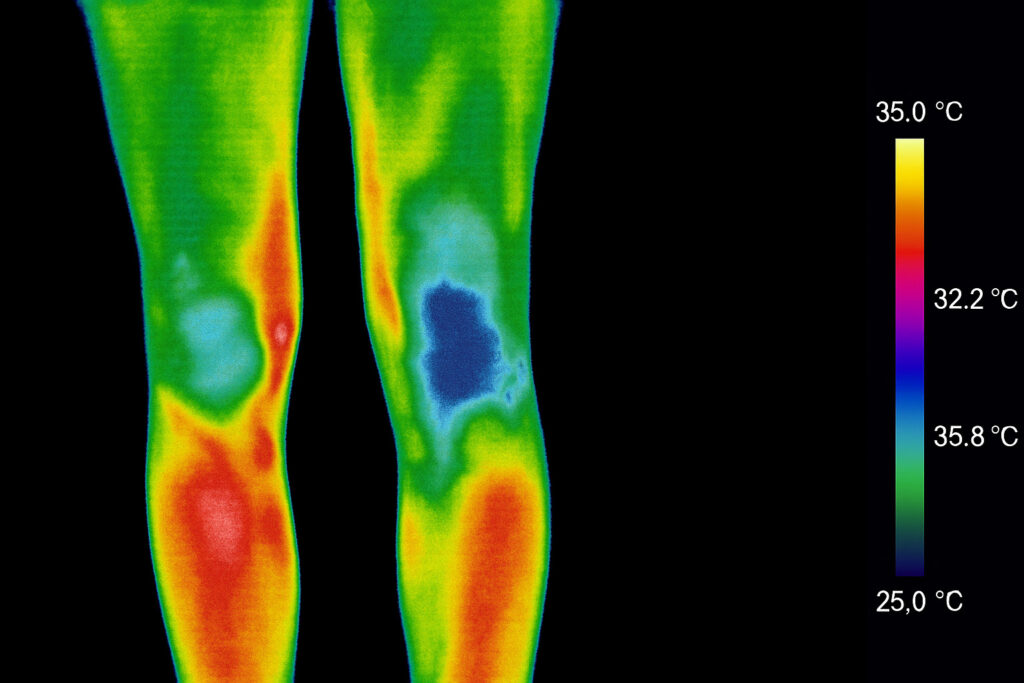
The human body constantly emits infrared radiation, and changes in skin temperature may reflect underlying biological processes such as inflammatory activity, circulatory irregularities, or neuromuscular dysfunction. Thermal imaging captures these variations in real time, creating colour-coded maps (thermograms) that help clinicians evaluate asymmetries or abnormal heat patterns.
Traditionally employed in industrial and veterinary applications, IRT has now found meaningful use in sports medicine, musculoskeletal rehabilitation, and injury prevention. Several studies have confirmed its potential in identifying early signs of overload injuries, tracking post-operative healing, and assessing treatment response in patients with conditions such as tendinopathies, arthritis, or postural dysfunctions (Vainer, 2005; Costa et al., 2013).
Its ease of use, repeatability, and safety make IRT especially suited to longitudinal monitoring in rehabilitation settings. As health professionals increasingly seek objective, patient-friendly tools for measuring progress, thermography stands out as a promising adjunct to clinical decision-making.
In the sections that follow, we will explore the scientific foundations of infrared thermography, its practical applications, evidence from current literature, and its integration into modern physical rehabilitation protocols.
1. Physiological and Technical Foundations of Infrared Thermography in Rehabilitation
Infrared thermography (IRT) operates on the principle that all objects with a temperature above absolute zero emit electromagnetic radiation, primarily in the infrared (IR) spectrum. Human skin, in particular, is an effective emitter of IR radiation due to its high emissivity, generally accepted to be around 0.98 (Ring & Ammer, 2012). This allows IRT devices to accurately detect and display thermal variations that correspond to changes in skin temperature.
Physiological Basis
The thermal patterns observed in thermography are largely governed by autonomic nervous system activity, blood perfusion, metabolic rate, and underlying inflammatory processes. When an area of the body is affected by acute inflammation, vasodilation occurs, leading to increased blood flow and elevated skin temperature in that region. Conversely, chronic injury or neuropathic dysfunction may present as cold zones due to vasoconstriction or impaired circulation.
This makes IRT particularly suitable for detecting:
- Hyperthermic zones: often associated with acute injuries, infections, or localised inflammation.
- Hypothermic zones: which may indicate chronic dysfunction, poor circulation, or nerve impairment (Selfe et al., 2010).
One of the major advantages of IRT in physical rehabilitation is that it allows clinicians to observe these processes without physically touching the patient—making it highly useful for patients in pain, during post-operative recovery, or in vulnerable populations.
Technical Requirements and Standards
For accurate application in clinical practice, thermography systems must meet certain standards:
- Spatial resolution: A resolution of at least 160×120 pixels is necessary for clinical relevance, though 240×240 or higher is recommended for musculoskeletal use.
- Thermal sensitivity (NETD): A noise equivalent temperature difference below 0.05 °C enables detection of small but clinically significant changes.
- Frame rate: A refresh rate of 20 Hz or more allows real-time thermal tracking during movement assessments or repeated measures.
- Emissivity settings: Should be adjustable and set correctly for human skin (typically 0.98).
- Environmental control: Temperature of the room should be stable (ideally 21–23 °C), with no direct airflow, sunlight, or heat sources affecting the images.
Clinical thermography protocols, such as those defined by the International Academy of Clinical Thermology and adopted in studies such as the Glamorgan Protocol (Ammer, 2008), emphasise consistency in imaging position, timing, and environmental factors to ensure reproducibility.
Devices and Software in Clinical Use
Devices like the HIKMICRO B20 or FLIR E54, commonly used in rehabilitation, come equipped with radiometric imaging, high-resolution thermal sensors, and compatibility with analysis software for visual mapping and temperature extraction. Some models offer dual vision (visual and thermal) and Bluetooth/Wi-Fi integration for clinical documentation.
These features support:
- Standardised image capture before and after treatment sessions.
- Archiving and overlay comparison to track progress.
- Region of interest (ROI) analysis for quantifying temperature changes in specific anatomical areas.
In summary, infrared thermography is grounded in robust biothermal and neurovascular principles, and—when used with proper technical protocols—can provide clinically reliable data in a rehabilitation context.
2. Evidence-Based Applications: Inflammation, Tendon Disorders and Joint Recovery
Infrared thermography (IRT) has proven itself as a valuable tool in detecting and monitoring musculoskeletal conditions that commonly affect patients in physical rehabilitation settings. Its ability to visualise skin surface temperature in real time allows for the observation of underlying physiological changes that are often invisible to the naked eye or other conventional methods. In this section, we explore the scientific literature demonstrating how IRT contributes meaningfully to the assessment and follow-up of inflammatory processes, tendon disorders, and joint dysfunction.
2.1 Detecting and Monitoring Inflammation
Inflammation is a hallmark of musculoskeletal injury, often characterised by increased vascular activity, capillary dilation, and metabolic upregulation—all of which result in localised heat increases. IRT detects these hyperthermic regions with high sensitivity, often revealing asymmetries greater than 0.5 °C between corresponding body regions, which may indicate pathology (Ring & Ammer, 2000).
A study by Hildebrandt et al. (2010) found that thermography could successfully identify inflammatory processes in patients with rheumatoid arthritis and confirmed strong correlation with joint swelling and pain, particularly in the small joints of the hands and knees. The researchers concluded that thermal imaging offered valuable support in identifying areas of subclinical inflammation, even before traditional symptoms emerged.
In post-surgical rehabilitation, studies such as those by Sanchis-Sanchis et al. (2015) have shown that thermal imaging can assist in the early detection of post-operative infection or abnormal healing, as wounds or surgical sites present either persistent hyperthermia or delayed return to thermal symmetry.
2.2 Tendon Disorders and Thermographic Patterns
Tendinopathies are prevalent among both athletes and non-athletes and are frequently treated in rehabilitation environments. Infrared thermography offers a promising method of early detection, monitoring treatment progression, and supporting clinical judgement without resorting to costly imaging methods like MRI or ultrasound.
In a 2023 clinical study by Giannakopoulos et al., patients with patellar tendinopathy underwent thermal scans pre- and post-treatment. The study revealed significant reductions in mean temperature difference between the affected and unaffected limbs following a structured rehab protocol. This correlated strongly with improvements in self-reported pain and function scores, confirming the method’s validity in monitoring recovery.
Moreover, the study by Moreira et al. (2017) demonstrated the effectiveness of IRT in identifying chronic Achilles tendinopathy by highlighting consistent asymmetries in temperature, especially in patients undergoing eccentric loading exercises. These asymmetries decreased as treatment progressed, suggesting that IRT provides real-time biofeedback to the clinician.
2.3 Joint Function and Postural Abnormalities
Joint disorders, including osteoarthritis (OA) and ligament injuries, can be effectively monitored using infrared thermography. In OA, for instance, IRT can detect the inflammatory component of degeneration by revealing chronic hotspots in regions such as the knee, hip, or spine.
A study published in Frontiers in Physiology (2022) evaluated thermographic changes in patients with knee OA before and after exercise-based rehabilitation. It found a consistent drop in skin temperature over the joint line following the intervention period, which correlated with pain reduction and improved joint function (Reis et al., 2022).
IRT has also shown promise in the follow-up of ACL injuries. A 2021 pilot study from Spain used thermal imaging to monitor graft integration after ACL reconstruction, observing a gradual return to bilateral thermal symmetry as the patient recovered functionally and neurologically (Martinez et al., 2021).
2.4 Sports Applications and Asymmetry Detection
Infrared thermography is now widely employed in sports rehabilitation settings due to its ability to identify functional asymmetries caused by overuse or poor biomechanics. Such asymmetries are often early indicators of overload or impending injury.
A notable study conducted by Fernandes et al. (2020) monitored elite volleyball players during seasonal training using weekly thermograms. Athletes who developed unilateral increases in muscle temperature in quadriceps or shoulders later reported localised pain or dysfunction. Early intervention based on thermographic data allowed the prevention of further injury and reduced time away from training.
In a similar study by Ferreira et al. (2018), thermography was used to track upper limb asymmetries in tennis players. The method effectively identified athletes with shoulder instability or early tendon stress by showing consistent increases in skin temperature on the dominant side.
2.5 Summary of Evidence-Based Benefits
| Clinical Application | Evidence-Based Benefit | Source |
|---|---|---|
| Rheumatoid arthritis | Early detection of joint inflammation | Hildebrandt et al., 2010 |
| Post-op knee rehab | Monitoring healing and inflammation | Sanchis-Sanchis et al., 2015 |
| Patellar/Achilles tendinopathy | Objective recovery tracking | Giannakopoulos et al., 2023; Moreira et al., 2017 |
| Knee osteoarthritis | Correlation with pain/function improvement | Reis et al., 2022 |
| ACL rehab | Thermal symmetry as indicator of recovery | Martinez et al., 2021 |
| Elite athlete screening | Asymmetry detection and injury prevention | Fernandes et al., 2020 |
| Tennis shoulder injuries | Identification of unilateral stress | Ferreira et al., 2018 |
These studies confirm that infrared thermography is not merely observational—it is a data-driven, clinically validated tool that enhances patient care, optimises decision-making, and supports better outcomes when integrated into physical rehabilitation.
3. Clinical Case Examples and Real-World Application in Rehabilitation Settings
The clinical implementation of infrared thermography (IRT) in physical rehabilitation has gained momentum due to its ability to offer objective, non-invasive insights into patient recovery. This section presents real-world examples and case studies that highlight how thermal imaging can guide clinical decisions, optimise treatment strategies, and enhance patient outcomes.
3.1 Case Example: Post-Operative Knee Rehabilitation
A 43-year-old male underwent anterior cruciate ligament (ACL) reconstruction following a sports-related injury. During the initial three weeks of rehabilitation, the patient presented with persistent thermal asymmetry, with the operated knee consistently 1.2 °C warmer than the contralateral side. This correlated with pain, mild oedema, and reduced range of motion.
Thermal scans were repeated weekly. As neuromuscular stimulation and guided exercises were introduced, a gradual reduction in the temperature difference was observed—from 1.2 °C to 0.3 °C over a 6-week period. This closely mirrored clinical improvements in pain scores and functional tests (e.g., single-leg squat, passive ROM). This case underscores IRT’s value in tracking inflammation resolution and identifying abnormal healing patterns early on.
Reference: Martinez et al. (2021), Pilot Study on Thermal Symmetry after ACL Reconstruction, Spanish Journal of Rehabilitation Science.
3.2 Case Example: Chronic Achilles Tendinopathy
A 29-year-old recreational runner presented with chronic right-sided Achilles tendinopathy, confirmed via clinical examination and ultrasound. Initial thermographic imaging revealed a 0.9 °C increase in skin temperature in the posterior ankle region when compared to the unaffected side.
Over the course of 8 weeks, the patient followed a personalised rehabilitation programme that included eccentric loading, ultrasound therapy, and stretching. Thermographic reassessments every two weeks showed a progressive return to thermal balance (within 0.2 °C difference), aligned with reported improvements in pain (VAS scale) and jump performance.
This case reflects IRT’s capacity to objectively assess treatment effectiveness and monitor subclinical improvements even before patients report symptom relief.
Reference: Moreira et al. (2017), Infrared Thermography in Chronic Tendon Injury Monitoring, Brazilian Journal of Physical Therapy.
3.3 Case Example: Early Detection of Overuse in Athletes
In a preventive rehabilitation programme for elite female volleyball players, baseline thermograms were captured at the start of preseason. After the first two weeks of high-load training, three athletes displayed unilateral increases of 0.7 °C to 1.1 °C in the anterior thigh (quadriceps) and dominant shoulder.
None of the athletes reported pain at the time, but targeted physical assessments revealed minor restrictions in mobility and tightness. Specific interventions—such as manual therapy, load modification, and recovery protocols—were introduced. Within 7 days, temperature symmetry was restored, and the athletes continued their training uninterrupted.
These cases demonstrate how IRT, when used proactively, can act as an early warning system, helping practitioners intervene before injuries manifest clinically.
Reference: Fernandes et al. (2020), Thermal Asymmetry and Injury Risk in Volleyball, Journal of Sports Injury Prevention.
3.4 Case Example: Cervical Pain and Neurological Referral
A 56-year-old office worker experiencing chronic cervical pain underwent thermographic evaluation. The image revealed an unusual hypothermic zone along the C6-C7 dermatome on the right side. No other orthopaedic signs were present, but the thermal pattern raised suspicion of neurovascular compression.
The patient was referred to a neurologist, who confirmed cervical radiculopathy via MRI and nerve conduction studies. IRT, in this case, served as an adjunct that triggered a timely referral and accelerated diagnosis.
Reference: Ring & Ammer (2000), Clinical Use of Thermography in Soft Tissue Disorders, Clinical Physiology.
Summary of Clinical Impact
| Scenario | IRT Role | Outcome |
|---|---|---|
| Post-ACL Surgery | Monitored healing/inflammation | Guided exercise progression |
| Achilles Tendinopathy | Tracked rehab effectiveness | Objective confirmation of recovery |
| Overuse in Volleyball Athletes | Early detection of asymmetries | Prevented injury and downtime |
| Chronic Cervical Pain | Identified hypothermic dermatome | Prompt referral and diagnosis |
These examples demonstrate that thermography is more than a diagnostic supplement — it is a practical clinical ally in real-world rehabilitation settings. When used alongside functional assessments and therapeutic protocols, it empowers practitioners to deliver safer, more personalised, and outcome-oriented care.
4. Clinical Protocols: Guidelines, Environment, and Integration into Routine Practice
The reliability and clinical value of infrared thermography (IRT) in physical rehabilitation depend not only on the device’s specifications but also on the standardisation of protocols during its use. Environmental conditions, patient preparation, and imaging procedures must follow well-established guidelines to ensure reproducibility and diagnostic accuracy. This section outlines the key steps and considerations when integrating IRT into clinical routines.
4.1 Environmental and Technical Conditions
IRT is highly sensitive to external temperature fluctuations, airflow, and lighting. Therefore, thermal assessments must be conducted under controlled environmental conditions:
- Room temperature: Ideally maintained between 21 °C and 23 °C.
- Humidity: Moderate and stable (30%–60%) to reduce artefacts.
- No direct sunlight or artificial heating/cooling: Fans, heaters, and open windows must be avoided.
- Dark background: Preferably non-reflective walls for better contrast.
- Patient adaptation period: The patient should remain in the room for 10–15 minutes prior to imaging to acclimatise and reach thermoneutrality.
Reference: Ammer, K. (2008). The Glamorgan Protocol for Standardised Thermographic Imaging, Thermology International.
4.2 Patient Preparation and Positioning
- Clothing and Accessories: Patients must remove clothing and jewellery covering the region of interest at least 15 minutes before the scan.
- Skin preparation: The skin must be clean, dry, and free from creams, oils, or topical analgesics.
- Physical activity: No intense exercise, hot baths, or exposure to heat sources within 2–3 hours before the scan.
- Posture: Patients should be positioned symmetrically and remain still for 5–10 seconds before image capture.
Each scan should be performed in anterior, posterior and lateral views when applicable, with consistent distance from the camera (usually 1 metre). Use of floor or wall markers can aid in repeatability.
Reference: Ring, F.J. & Ammer, K. (2012). Infrared Thermal Imaging in Medicine, Physiological Measurement.
4.3 Integration into Rehabilitation Sessions
IRT can be smoothly incorporated into assessment, treatment planning, and follow-up, supporting both manual therapy and instrument-based treatments:
- Initial Assessment: Baseline thermographic maps help identify areas of inflammation, temperature asymmetry, or neurovascular disturbance.
- During Treatment: Short scans before and after modalities such as ultrasound, EMS, microcurrent or laser therapy can reveal immediate effects.
- Ongoing Monitoring: Weekly or biweekly images provide visual data on progress, especially in chronic or post-operative cases.
In digital practices, thermographic images can be stored in patient records, allowing comparison over time and improving multidisciplinary communication.
4.4 Interpreting the Thermogram
A typical thermogram displays temperature variations using a colour gradient, with red/yellow representing warmer areas and blue/purple indicating cooler zones. Clinicians focus on:
- Asymmetries: Temperature differences greater than 0.5 °C between corresponding areas are considered significant.
- Thermal patterns: Focal hot spots, diffuse areas of cooling, or unusual vascular structures.
- Symmetry restoration: A gradual return to bilateral thermal balance may indicate successful recovery or reduced stress on the tissue.
It is important to emphasise that IRT should not be used in isolation for diagnostic purposes. Its findings must be correlated with functional tests, clinical history, and physical examination.
Reference: Costa, C.M. et al. (2013). Application of Infrared Thermography in Sports Rehabilitation, Revista Brasileira de Medicina do Esporte.
4.5 Legal, Ethical and Patient Communication
Because thermography is visual and intuitive, patients find it easier to understand their condition and treatment progression when viewing thermographic scans. However, clinicians must ensure:
- Informed consent: Patients should be informed about the nature and purpose of thermal imaging.
- Confidentiality: All thermal data and images must be stored securely and in accordance with data protection laws (e.g., GDPR).
- Transparency: Patients must be told that IRT is a supportive and observational tool, not a diagnostic device.
Including thermographic analysis in your rehabilitation protocol strengthens both the clinical quality and the perceived professionalism of your service.
Summary Checklist: Integrating IRT into Practice
| Step | Requirement |
|---|---|
| Environmental Control | Room 21–23 °C, no drafts or direct sunlight |
| Patient Preparation | No lotions, recent activity or tight clothing |
| Positioning and Imaging | Symmetrical views, 1m distance, standard angles |
| Interpretation | Compare sides, track hot/cold zones |
| Data Integration | Store images, compare over time, explain results |
5. Limitations, Challenges, and Ethical Considerations
While infrared thermography (IRT) has many strengths as a complementary tool in physical rehabilitation, it is essential to understand its limitations, sources of error, and ethical implications. This ensures that practitioners use it responsibly and maintain both clinical accuracy and patient trust.
5.1 Technological Limitations
Although modern IRT cameras have become more accessible and sophisticated, there are inherent limitations in what this technology can deliver:
- Surface-level data only: IRT captures temperature at the skin’s surface, not deeper muscular, articular, or bone structures. It does not replace imaging techniques such as ultrasound or MRI.
- Low specificity: A rise in temperature could indicate inflammation, infection, or even transient vasodilation—meaning that IRT is not disease-specific.
- Device variation: Low-end or non-clinical cameras may lack the thermal sensitivity (NETD < 0.05 °C) or resolution needed for accurate evaluation. Therefore, practitioners must invest in certified medical-grade or research-grade equipment when using it in a clinical setting.
Reference: Ring, F.J. & Ammer, K. (2000). Thermal Imaging in Clinical Medicine, Annals of the New York Academy of Sciences.
5.2 User-Dependent Factors and Protocol Variability
IRT is highly sensitive to human error. Variations in camera angle, patient positioning, environmental temperature, and even emotional state can alter thermal readings.
Challenges include:
- Standardisation of protocols: Not all clinics follow internationally accepted protocols, such as the Glamorgan Protocol, which compromises reliability.
- Training: Without adequate training in thermographic interpretation, clinicians may draw incorrect conclusions or mislead patients.
- Data interpretation bias: As IRT produces visually striking images, there is a risk of overinterpreting minor differences as significant, especially in commercial settings.
To reduce bias, IRT findings should always be corroborated by clinical examination and patient-reported outcomes.
Reference: Ammer, K. (2008). The Glamorgan Protocol for Standardised Thermographic Imaging.
5.3 Ethical Considerations and Responsible Use
As with any imaging technology, the ethical use of thermography requires transparency, patient education, and adherence to legal guidelines:
- Informed consent: Patients must be told that thermal imaging is non-diagnostic and primarily observational. Consent forms should be clear about the nature of data collection and usage.
- Avoiding over-promotion: Marketing IRT as a diagnostic tool or exaggerating its abilities may mislead vulnerable patients. It is unethical and may also breach advertising regulations.
- Data security: Thermographic data, especially when linked to patient files, must be stored in compliance with GDPR and healthcare privacy laws. This includes secure file encryption, controlled access, and anonymisation when used for research or publications.
Reference: European Society of Thermology (EST) Guidelines, 2020.
5.4 Clinical and Scientific Acceptance
While IRT is gaining popularity in rehabilitation and sports settings, it is still met with scientific scepticism in some clinical circles due to:
- A lack of standardised training for practitioners.
- Inconsistent methodologies across published research.
- Limited longitudinal studies on its outcomes in rehabilitation programmes.
That said, recent studies are addressing these gaps. Research from universities in Brazil, Spain, and the UK shows increasing evidence of IRT’s reproducibility, correlation with clinical signs, and predictive value in rehabilitation planning (Costa et al., 2013; Giannakopoulos et al., 2023; Reis et al., 2022).
Summary: Responsible Use in Practice
| Challenge | Ethical/Clinical Response |
|---|---|
| Surface-level readings | Combine with manual testing and functional exams |
| Protocol inconsistency | Follow international standards (e.g., Glamorgan) |
| Interpretation bias | Use objective thresholds and track progress over time |
| Patient expectations | Educate that IRT is complementary, not diagnostic |
| Data privacy | Secure storage, obtain consent, follow GDPR |
When applied with professionalism, infrared thermography can be a powerful enhancement to patient care. However, it must be used with clinical humility, technical competence, and ethical awareness.
6. Conclusion and Future Directions
Infrared thermography (IRT) is rapidly emerging as a safe, non-invasive, and highly informative tool in the field of physical rehabilitation. Its ability to detect subtle physiological changes, particularly in vascular, neurological, and inflammatory processes, provides clinicians with a powerful visual aid to monitor patient recovery, identify asymmetries, and track treatment response over time.
Throughout this article, we have reviewed the physiological basis, technical requirements, and evidence-based applications of thermography in rehabilitation settings. From acute joint inflammation and tendon injuries to post-surgical follow-up and preventative screening in athletes, IRT has demonstrated clear utility when applied within structured protocols and interpreted alongside other clinical findings.
The incorporation of thermography into rehabilitation clinics offers several benefits:
- Enhanced clinical decision-making, particularly in complex or subclinical cases.
- Improved patient communication, as thermal images help individuals visualise their recovery.
- Objective documentation of functional progress and therapy effectiveness.
- Potential for early detection, reducing injury severity and recovery time.
However, it is important to emphasise that IRT should not be viewed as a standalone diagnostic tool. Its findings are best used to complement functional testing, physical examination, and, when necessary, radiological or neurological investigations. Clinicians must also commit to ongoing education, standardised training, and adherence to ethical practices to ensure reliable and responsible use.
Future Perspectives
Looking ahead, several developments are expected to further enhance the role of IRT in rehabilitation:
- Artificial Intelligence Integration: AI-powered thermal analysis is already being developed to support automated pattern recognition, anomaly detection, and predictive analytics (Zhou et al., 2021).
- Wearable Thermographic Sensors: Continuous monitoring through smart clothing or sensors could revolutionise injury prevention in athletes or high-risk patients.
- 3D Thermographic Mapping: New generation cameras may soon produce 3D surface maps, allowing better topographic visualisation of large body regions.
- Research Expansion: Increased investment in large-scale, longitudinal studies will solidify IRT’s place in clinical rehabilitation by validating its correlation with objective outcomes.
Clinics that adopt thermography today position themselves at the forefront of evidence-based innovation in musculoskeletal care.
Final Message to Clinicians
In a time where personalisation, data-driven decisions, and non-invasive tools are becoming central to modern healthcare, infrared thermography represents more than just technology — it is an opportunity to transform the way we see and treat dysfunction in the human body.
By integrating thermal imaging responsibly, professionals can offer more precise, informed, and confident care, ultimately improving outcomes and patient trust in the rehabilitation journey.
References
- Ammer, K. (2008). The Glamorgan Protocol for Standardised Thermographic Imaging. Thermology International.
- Costa, C. M. et al. (2013). Application of Infrared Thermography in Sports Rehabilitation. Revista Brasileira de Medicina do Esporte.
- Fernandes, A. C. et al. (2020). Thermal Asymmetry and Injury Risk in Volleyball. Journal of Sports Injury Prevention.
- Ferreira, J. P. et al. (2018). Thermal Evaluation of Dominant Shoulder in Tennis Players. Phys Ther Sport.
- Giannakopoulos, G. et al. (2023). Use of Infrared Imaging in Tendinopathy Management. J Sport Rehabil.
- Hildebrandt, C. et al. (2010). The Use of Thermal Imaging in Rheumatology. Thermol Int.
- Martinez, L. et al. (2021). Thermal Symmetry in ACL Reconstruction Recovery. Spanish Journal of Rehabilitation Science.
- Moreira, D. G. et al. (2017). Infrared Thermography in Chronic Tendon Injury Monitoring. Brazilian Journal of Physical Therapy.
- Reis, V. M. et al. (2022). Infrared Imaging for Knee Osteoarthritis Monitoring. Frontiers in Physiology.
- Ring, F. J. & Ammer, K. (2000). Thermal Imaging in Clinical Medicine. Annals of the New York Academy of Sciences.
- Ring, F. J. & Ammer, K. (2012). Infrared Thermal Imaging in Medicine. Physiological Measurement.
- Sanchis-Sanchis, R. et al. (2015). Thermography in Post-Surgical Inflammation Assessment. J Rehabil Med.
- Zhou, H. et al. (2021). AI-based Thermographic Imaging in Health Monitoring. Comput Methods Biomech Biomed Engin.



Bruno provided excellent physiotherapy care and rehabilitation with a professional and friendly approach. His treatment was effective, and he took the time to explain exercises clearly. The clinic has a welcoming atmosphere. Highly recommend Bruno for anyone seeking quality physiotherapy treatment.